

In general, if 50% of the calculated shock volume of isotonic crystalloid has not caused sufficient improvement, consider either switching to or adding a colloid.

Patients may be hypovolemic, dehydrated, hypotensive, or a combination of all three. High K administration rates may lead to cardiac arrest therefore, do not exceed 0.5 mmol/kg/hr. If electrolytes such as K are needed in the emergent situation, administer through a second IV catheter. IV isotonic crystalloid fluids are the initial fluid of choice. When intravascular volume expansion without whole blood is needed, use crystalloids, colloids, or both. 2 mmol/L).20–22 Note that cats in hypovolemic shock may not be tachycardic. Hypovolemia due to decreased oncotic pressure is suspected in patients that have a total protein, 35 g/L (3.5 g/dL) or albumin, 15 g/L (1.5 g/dL).19 Patients in shock may have hypovolemia, decreased BP, and increased lactate (. Hypovolemic patients have signs of decreased tissue perfusion, such as abnormal mentation, mucous membrane color, capillary refill time, pulse quality, pulse rate, and/or cold extremity temperature. Hypotension is discussed under “Fluids and Anesthesia.”Ĭommon causes of hypovolemia include severe dehydration, rapid fluid loss (gastrointestinal losses, blood, polyuria), and vasodilation. Hypotension may exist separately or along with hypovolemia and dehydration (Figure 1). Hypovolemia and dehydration are not mutually exclusive nor are they always linked. Dehydration is the depletion of whole body fluid. Hypovolemia refers to a decreased volume of fluid in the vascular system with or without whole body fluid depletion.
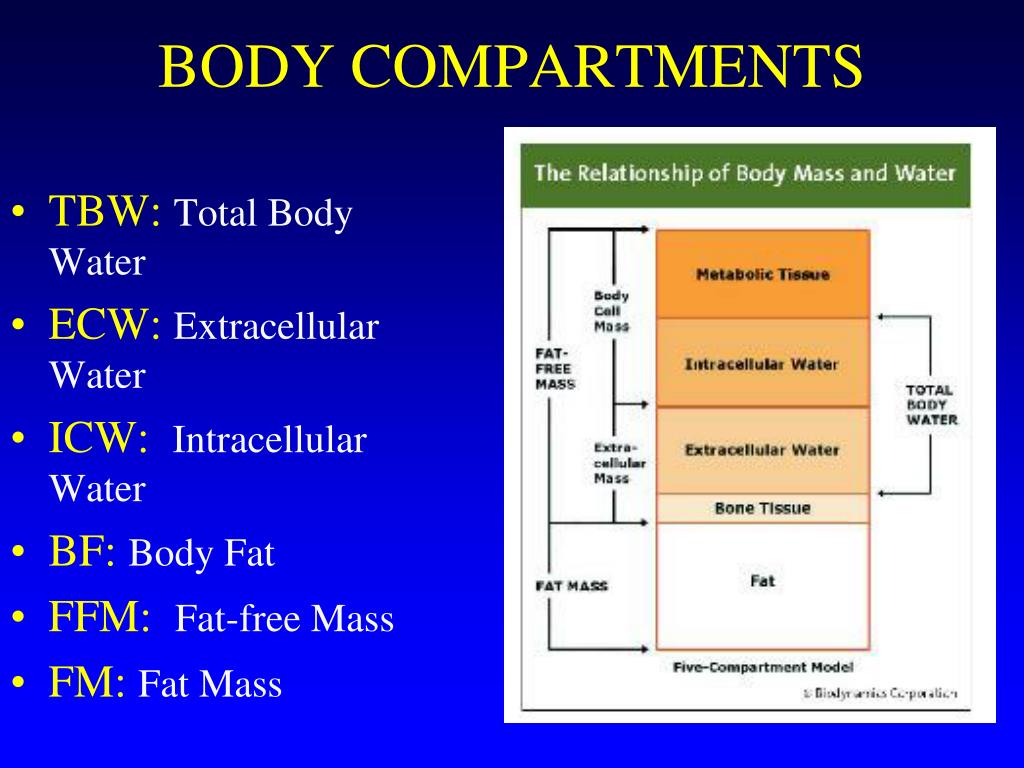
The body fluid compartments change skin#
Moderate loss of skin turgor, dry mucous membranes, weak rapid pulses, enophthalmosĬonsiderable loss of skin turgor, severe enophthalmos, tachycardia, extremely dry mucous membranes, weak/thready pulses, hypotension, altered level of consciousness 50 Minimal loss of skin turgor, semidry mucous membranes, normal eye * Not all animals will exhibit all signs. Maintenance solutions low in Na should not be used to replace extracellular deficits (to correct dehydration) because that may lead to hyponatremia and hyperkalemia when those solutions are administered in large volumes.Assess for euhydration, and avoid fluid overload through monitoring for improvement. Frequency of monitoring will depend on the rate at which fluid resuscitation is being administered (usually q 15–60 min).The typical goal is to restore euhydration within 24 hr (pending limitations of comorbid conditions such as heart disease). Replace ongoing losses within 2–3 hr of the loss, but replace deficit volumes over a longer time period. Add the deficit and ongoing losses to maintenance volumes.General principles for fluid therapy to correct dehydration include the following: Estimating the percent dehydration gives the clinician a guide in initial fluid volume needs however, it must be considered an estimation only and can be grossly inaccurate due to comorbid conditions such as age and nutritional status (Table 5).īody weight (kg)3 % dehydration ¼ volume (L) to correct


 0 kommentar(er)
0 kommentar(er)
